Electronic Medical Records (EMRs): Pros, Cons, and Considerations for Healthcare Leaders
Electronic Medical Records (EMRs) have played an important role in the healthcare technology landscape for several decades. For CIOs and other senior executives in healthcare organizations, understanding the benefits and drawbacks of EMRs is essential to making informed decisions about digital transformation.
In most cases, you are probably already using or connected to an EMR, depending on your organization's role in the healthcare market. However, you might be considering switching to a new provider, or plugging-in different systems. So it's important to consider how you use an EMR and whether you're currently using the right one.
In this article, we provide an in-depth look at what EMRs are, EMR pros and cons, contrasting them with Electronic Health Records (EHRs), and discussing how to determine if EMRs are the right choice for your organization.
What Are Electronic Medical Records (EMRs)?
Electronic Medical Records (EMRs) are digital versions of the paper charts and physical healthcare records of patients. They contain the medical and treatment history of patients and are designed to support diagnosis and treatment.
The use of EMRs dates back to the 1960s, with more widespread adoption starting around the time of the first Dot-com boom, in the early 2000s. This also coincided with the Clinton administration's implementation of the Health Insurance Portability and Accountability Act (HIPAA) in 1996.
According to a recent study, the EMR market will be worth $11.3 billion globally by 2034. One country, New Zealand, has already achieved 100% full adoption from paper to digital healthcare records.
Unlike traditional paper records, EMRs facilitate the digital storage, retrieval, and management of patient data. This can include medical history, diagnoses, medications, immunization dates, allergies, lab results, and imaging studies. Healthcare professionals and anyone with access should be able to find out everything they need to know about a patient through an EMR.
The Role of EMRs in Healthcare
EMRs are integral to modern healthcare for several key reasons:
- Improved Accuracy: Digital records reduce the risk of misinterpretation and mistakes that may arise from the famously illegible handwriting of doctors and provide standardized information that can be easily updated for nurses and other healthcare staff.
- Enhanced Efficiency: With immediate access to patient information, healthcare professionals can make quicker, more informed decisions, leading to better patient outcomes. This is also better for insurance firms, payers, and patients themselves.
- Streamlined Workflow: Most EMRs integrate seamlessly with other digital tools, such as lab systems and radiology. This can create a unified ecosystem that minimizes redundant processes and duplications.
- Data Analytics and Research: EMRs allow for the aggregation of large amounts of data, which can be analyzed to identify trends, measure treatment outcomes, and inform evidence-based practices.
- Regulatory Compliance: Many healthcare regulations and standards are designed around the digital collection and management of patient data, making EMRs essential for compliance and reporting. This is especially true of HIPAA, so no EMR is worthy of the name if it's not HIPAA compliant.
Now, let's look at Electronic Medical Records pros and cons, starting with 10 upsides of using an EMR.
10 Pros of EMRs
Implementing an EMR system can offer numerous benefits. Here are 10 of the most common advantages of using EMRs:
-
Improved Patient Care
- Comprehensive Data Access: EMRs give healthcare providers immediate access to a patient's complete medical history, which can be critical in emergencies. This enables more accurate diagnoses and timely treatments. This further results in better patient and healthcare outcomes, which is the ultimate goal of every treatment.
- Better Coordination: EMRs improve communication among multidisciplinary teams, ensuring that every provider has access to the most recent patient information. This prevents mistakes and can make the difference between life and death, a healthy patient, or a lawsuit.
-
Enhanced Efficiency and Productivity
- Faster Data Retrieval: Digital records eliminate the time spent searching for paper documents, allowing providers to focus more on patient care rather than admin work. This also reduces costs and the need to hire as many admin staff.
- Automated Workflows: EMRs support automated tasks such as appointment scheduling, billing, and reminders for preventive care, which enhances overall operational efficiency. They have become even more efficient thanks to recent AI integrations.
-
Increased Accuracy and Reduced Errors
- Standardized Documentation: EMRs use structured data fields and templates that minimize the risk of human error. Automated alerts and reminders can flag potential drug interactions or allergies. Input fields can be modified according to the processes of healthcare providers and who needs access to these records.
- Real-Time Updates: Information is updated instantly, keeping all healthcare providers working with the most up-to-date patient data.
-
Enhanced Patient Engagement
- Patient Portals: Many EMR systems include patient portals that allow individuals to access their own health records. This makes it easier for patients to review test results and communicate with their providers, promoting active participation in their care.
- Transparency and Trust: Easy access to personal health information can build trust and improve the overall patient experience. It also means that patients don't need to call medical reception desks to get the information they need, thereby keeping operational costs low.
-
Facilitated Data Analysis and Research
- Population Health Management: EMRs allow for the aggregation of data across patient populations, enabling healthcare organizations to track trends, measure treatment outcomes, and identify areas for improvement.
- Clinical Research: The wealth of data contained in EMRs can be invaluable for clinical studies and research, bringing advancements in medical knowledge and treatment protocols.
-
Cost Savings Over Time
- Reduction in paper records and letters: Transitioning from paper-based records to digital records reduces the costs associated with printing, storage, and document management.
- Streamlined administrative processes: AI and Automation reduces the need for as many labor-intensive admin tasks. This increased efficiency allows staff to focus on higher-value activities, which can lead to long-term cost savings.
-
Improved Regulatory Compliance
- Audit Trails: EMRs provide detailed audit trails that track who accessed a patient's records and when. Data audit trails increase security and are essential for meeting regulatory requirements.
- Standardized Reporting: Digital records simplify the process of generating reports for government agencies and other oversight bodies.
-
Enhanced Security and Data Backup
- Controlled Access: EMRs offer role-based access control, making sure that only authorized personnel can access sensitive patient data. This is one of the cornerstones of HIPAA and other digital healthcare laws.
- Data Backup: Digital records are typically backed up regularly, reducing the risk of data loss due to physical disasters or human error.
-
Better Coordination of Care
- Interoperability: Many modern EMR systems are designed to integrate with other healthcare IT systems, such as lab information systems and radiology, facilitating a more cohesive patient care process.
- Continuity of Care: In cases where patients see multiple specialists, EMRs provide all healthcare providers with access to the most current patient information, helping to prevent unnecessary tests and avoid conflicting treatments.
-
Environmental Benefits
- Reduced Paper Waste: The shift to digital records significantly cuts down on paper usage, contributing to environmental sustainability.
- Lower Carbon Footprint: Digital storage and electronic communication reduce the need for physical transport and storage, further decreasing the organization's environmental impact.
At the same time, there are downsides to think about too.
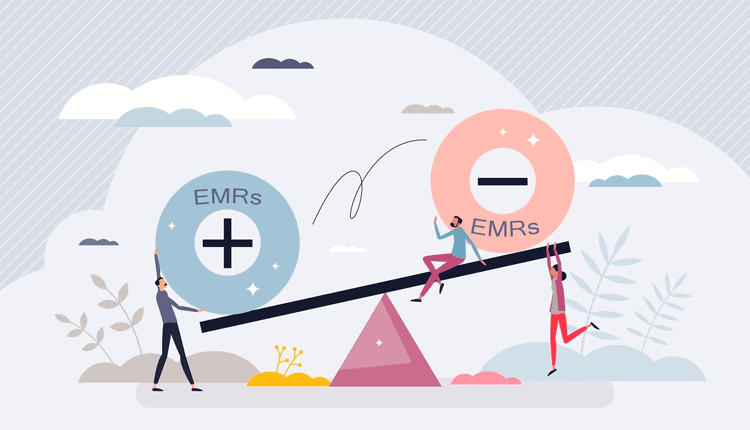
10 Cons of EMRs
Despite the many benefits, EMRs also come with challenges that organizations must consider carefully:
-
High Initial Costs
- Implementation Expenses: The initial cost of purchasing and installing an EMR system can be substantial. This includes not only the software but also necessary hardware upgrades.
- Training Costs: Staff must be trained on the new system, which requires time and financial investment.
-
Ongoing Maintenance and Upgrades
- Continuous Investment: EMR systems require regular updates and maintenance to keep them secure and functional. This ongoing cost can strain budgets, especially for smaller organizations.
- System Upgrades: Keeping the system current with the latest technology and regulatory standards can necessitate frequent upgrades.
-
Potential for Workflow Disruption
- Transition Challenges: Shifting from paper-based systems to digital records can initially disrupt established workflows. Staff may experience temporary slowdowns as they adapt to new processes.
- User Resistance: Change management is a significant challenge. Some staff may be resistant to adopting new technologies, preferring familiar paper records.
-
Data Security Concerns
- Cybersecurity Risks: While EMRs can enhance security through controlled access, they are also attractive targets for cybercriminals. Data breaches can expose sensitive patient information and lead to significant legal and financial repercussions.
- Compliance With Privacy and Healthcare Laws: Maintaining system compliance with regulations such as HIPAA (and the equivalent in other countries, if you operate outside of the US) can be complex and requires robust security measures.
-
Interoperability Issues
- System Compatibility: Not all EMR systems are designed to work seamlessly with other health IT systems. You need to avoid the danger of data silos and communication breakdowns between different departments or organizations. Make sure you have EMR software that plays well with other systems via plugins and APIs.
- Vendor Lock-In: Organizations may become dependent on a single vendor's system, making it challenging to switch providers or integrate new technologies. Lock-in periods can be 3-years if not longer, so you need to be careful about picking the right EMR supplier.
-
Data Entry and Documentation Challenges
- Time-Consuming Documentation: In some cases, the digital documentation process can be more time-consuming than traditional methods, potentially leading to longer patient visit times.
- User Interface Issues: Poorly designed interfaces can hinder efficiency, causing frustration among clinicians and increasing the likelihood of documentation errors.
-
Risk of Data Loss and Technical Failures
- System Downtime: Like any cloud-based system, EMR software can experience technical issues and downtime. In the event of a system failure, patient care could be compromised if there are not robust backup systems in place. This is also crucial to avoid litigation and fines in the event of a cyberattack.
- Data Migration Issues: Moving data from an old system to a new one can be challenging, with potential risks such as data loss or corruption during the migration process.
-
Complexity and Customization Difficulties
- Customization Needs: Each healthcare organization has unique needs. Off-the-shelf EMR solutions may not fully align with an organization's specific requirements, necessitating costly customization.
- Complexity of Use: The more features an EMR system has, the steeper the learning curve. Complex systems may require extensive training, which can delay the benefits of implementation.
-
Impact on Patient-Provider Interaction
- Screen Time vs. Face Time: A reliance on digital systems during consultations can sometimes detract from the personal interaction between patients and providers. Doctors and nurses may spend more time looking at screens than engaging with patients, potentially impacting the quality of care.
- Distracted Consultations: The need to input data during consultations might lead to interruptions in patient communication, affecting the overall patient experience. AI is now making this easier as inputting information is becoming more automated.
-
Legal and Regulatory Risks
- Audit and Compliance Pressure: With detailed audit trails and digital documentation, healthcare organizations must be careful when it comes to data accuracy and regulatory compliance. Mistakes can lead to legal liabilities and penalties.
- Litigation Risks: Inaccurate or incomplete digital records can serve as grounds for malpractice claims if errors in documentation contribute to negative and even dangerous patient outcomes.
Now, let's compare the differences between EMRs and EHRs (Electronic Health Records).
EMRs vs. EHRs: Understanding the Difference
While the terms Electronic Medical Record and Electronic Health Record are often used interchangeably, they refer to different systems that serve distinct purposes:
-
Electronic Medical Records (EMRs)
As we've covered here, EMRs are digital versions of paper charts in a clinician's office. They contain the medical and treatment history of patients within one healthcare provider.
EMRs can also be shared across different organizations, and with insurers, depending on what's required and the permissions granted.
EMRs are excellent for tracking data over time, identifying patients for preventive screenings, and monitoring overall performance.
-
Electronic Health Records (EHRs)
In contrast, Electronic Health Records (EHRs) extend beyond basic clinical data gathered in a provider's office and are specifically designed to be shared among different healthcare providers.
Compared to EMRs, EHRs can include a more comprehensive view of a patient's care, integrating data from multiple sources such as specialists, laboratories, and pharmacies.
Understanding the distinction is important because while EMRs are beneficial within a single setting, EHRs provide a more holistic view of patient health across various providers. The choice between implementing an EMR or EHR system — or a hybrid solution — depends largely on the organization's goals, infrastructure, and patient care models.
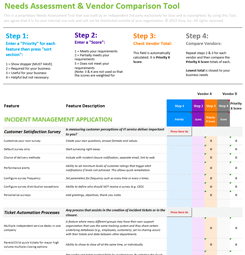
Determining if EMRs Are Worth It for Your Organization
Before investing in an EMR system, healthcare organizations must carefully evaluate several factors. Here are key considerations for decision-makers:
-
Organizational Readiness
Assess whether your organization has the technical infrastructure and IT support necessary to implement and maintain an EMR system. This includes hardware, network capabilities, and cybersecurity measures. These could be managed in-house or outsourced, providing you have the capabilities.
At the same time, remember that this is as much about user adoption as technological capabilities. Evaluate the willingness and ability of your staff to adapt to new technologies. Successful implementation requires comprehensive training programs and a culture that embraces change.
-
Financial Considerations
Costs and finances always have to factor into this. Conduct a cost-benefit analysis that considers both the upfront costs of installation and training, as well as the potential for long-term savings through increased efficiency and reduced operational costs.
Explore potential funding sources, grants, or incentives that may be available to help offset the costs of transitioning to a digital system.
-
Impact on Patient Care
Quality of care improvements have to be front-of-mind when making changes like this. Consider how an EMR system might enhance patient care through better data accuracy, improved care coordination, and streamlined processes.
Evaluate whether the implementation of an EMR system could improve patient engagement and satisfaction, potentially leading to better health outcomes and higher patient retention rates. If an EMR has proven to be beneficial to other healthcare organizations it could have the same positive effect on your organization.
-
Regulatory and Compliance Requirements
Ensure that the chosen EMR system complies with local, national, and international regulations related to patient data privacy and security. This should come as standard with any EMR system that would pass commercial healthcare purchasing requirements.
-
Future-Proofing and Scalability
Assess whether the EMR system can scale with your organization's growth and adapt to future technological advancements or regulatory changes.
At the same time, consider the system's ability to integrate with other digital health solutions, such as telemedicine platforms, EHR systems, and patient engagement tools.
-
Stakeholder Involvement
During any trial phase, involve healthcare and administrative staff in the decision-making process. This front-line input can provide valuable insights into what features are necessary for a smooth transition and ongoing success. Also, consider patient feedback regarding digital solutions. Patient satisfaction is also going to be an important measurement of the system's overall success.
-
Risk Management and Contingency Planning
Evaluate the vendor's security protocols and if they have robust measures in place to protect against an ever-growing number of cyber threats against healthcare providers.
During any trial or testing phase, develop a comprehensive plan for system downtime or data migration challenges, preventing patient care from being compromised during technical failures.
-
Competitive Advantage
Consider how a cost and time-effective EMR system might position your organization competitively. Enhanced operational efficiency and improved patient care can serve as differentiators in a competitive healthcare market.
EMRs: Pros and Cons Key Takeaways
Electronic Medical Records can streamline administrative tasks, enhance patient care, and provide a wealth of data for clinical decision-making and research.
For CIOs and senior healthcare leaders, the decision to adopt EMRs involves weighing significant benefits — such as improved patient outcomes, enhanced operational efficiency, and better data security — against challenges like high initial costs, potential workflow disruptions, and cybersecurity risks.
While the EMR system represents a powerful tool for improving healthcare delivery within a single organization, understanding its limitations and comparing it to the broader capabilities of EHR systems is critical.
As healthcare continues to evolve, staying ahead of innovations and adapting to new digital solutions will be key to sustaining competitive advantage and delivering exceptional patient care.
Useful EMR Resources
- HIPAA Resource Center
- HIPAA Compliant Solutions for Healthcare
- Healthcare Technology Industry Whitepapers
- Hospital Automation Fully Examined: Benefits and 12 Innovative Ways to Implement
How Giva Can Help with EMRs
EMR systems are powerful and useful pieces of medical software. If you aren't already using one, then it could be an option in the near to mid-term.
Giva provides, and has done for decades, a suite of HIPAA-compliant software solutions that support healthcare entities, such as hospitals, clinics, behavioral and mental health, healthcare software vendors and 3rd-party service providers.
All of these — Giva's IT Service Management, IT Help Desk, and Customer Service — support and interact with EMRs and EHRs. Data can be transferred between our HIPAA and HITECH-compliant software to transform and upgrade your customer, IT, patient, and healthcare experience.
For more, get a free demo to see Giva's solutions in action, or start your own free, 30-day trial today!