Change Management in Healthcare: How to Implement and Measure for Success
Change management in healthcare is complicated, multi-faceted, and impacts multiple user groups and stakeholders, including and especially healthcare providers and patients.
Because healthcare is a rigorously regulated and monitored sector, change management in healthcare has to be carefully monitored and managed.
Change management can be initiated from a number of different sources:
- Leadership-driven
- Regulatory
- Patient-centric
- Payer-driven
- Technological innovations (like AI or telehealth)
IT Service Management (ITSM) are usually the ones responsible for implementing and delivering change management, working with the relevant stakeholders and organizational leaders.
In this article, we look at the following in-depth:
- 6 challenges healthcare organizations usually face when implementing change management
- 10 most popular change management models and examples
- Top 5 best practices for healthcare organizations when implementing change management
- How to measure the impact of change management
Read on to find out everything you need to know about change management in healthcare.
What is Change Management in Healthcare?
Change management in healthcare refers to the structured approach of transitioning ITSM teams, and organizations from current operational approaches to new, more modernized ones.
ITSM teams or third-party vendors — including those that provide integrated IT services for healthcare providers — are usually guided by an Information Technology Infrastructure Library (ITIL®) framework.
In ITIL, change management, also known as change enablement is: "The addition, modification, or removal of anything that could have a direct or indirect effect on services."
The reason for using ITIL frameworks in ITSM change management is to: "Maximize the number of successful IT changes by ensuring that risks have been appropriately assessed, authorizing changes to proceed, and managing the Change Schedule."
ITSM change management involves planning, executing, and reinforcing changes to bring successful adoption while minimizing resistance and disruptions to healthcare delivery.
Having a structured approach to making technical changes is critical in the healthcare sector where technological advancements, regulatory updates, and evolving patient expectations demand constant adaptation.
Effective ITSM change management in healthcare helps make sure that changes:
- Are embraced by ITSM and the relevant patient-focused staff
- Are aligned with organizational goals
- Lead to improvements in patient care
- Lead to improvements in operational efficiency
- Promote better regulatory compliance (e.g., HIPAA).
Healthcare leaders must focus on people, processes, and technology to drive sustainable change. This is whether you are implementing a new electronic health record (EHR) system, adopting telehealth, or integrating AI into diagnostic processes.
When these changes are being driven or at least implemented by an ITSM team or provider it benefits everyone if they're being done using an ITIL structure.
6 Challenges in Healthcare Change Management
Healthcare organizations have to handle far more regulatory burdens than most businesses in any other sector. As a result, the challenges leaders face when trying to implement any kind of change are different than you might find elsewhere.
Not only that, because front-line staff are healthcare professionals — doctors, nurses, consultants, specialists, etc. — any top-down changes are usually viewed with skepticism.
Healthcare organizations face unique challenges when managing change, including:
- Resistance to Change: Healthcare professionals often resist new workflows or technologies due to fear of disrupting established routines, increased workload, or concerns about patient safety. Healthcare workers have heavy workloads already, and patient safety is always their top priority. You need to clearly show them that any changes, especially anything done in the name of "efficiency", aren't going to result in negative consequences for patients.
- Complex Regulations: Adapting to frequent regulatory updates can complicate change initiatives and require additional training. There are dozens of regulations governing every aspect of healthcare, including HIPAA. Make sure any changes and new technologies are fully covered under the relevant regulations.
- Resource Constraints: Although most healthcare organizations are usually worth billions, there are often constraints on resources. This impacts change management because limited budgets, staffing shortages, and competing priorities can hinder change management efforts.
- Interdisciplinary Collaboration: Maintaining alignment among various departments and stakeholders, including clinicians, administrative staff, and IT teams, can be difficult. If the changes being made are widespread, set up an interdisciplinary task force to spearhead the collaboration.
- Maintaining Patient Care Quality: For healthcare professionals, this is the most important consideration. Implementing change without disrupting patient care requires careful planning and execution.
- Technological Challenges: Integrating new digital tools or platforms into legacy systems often leads to technical and operational hurdles. Healthcare IT is made up of dozens of complex layers of technology. Anything new, or anything replacing something old needs to undergo an assessment as to how it will integrate with other systems.
10 Common Change Management Models and Examples in Healthcare
Change management models provide frameworks to guide healthcare organizations through ITSM and digital transitions. Using an ITIL-based framework makes it easier to implement any kind of digital changes within a healthcare setting.
The following 10 models and examples are highly effective in healthcare settings:
-
The ADKAR Change Management Model
The Prosci ADKAR® model (Awareness, Desire, Knowledge, Ability, and Reinforcement) focuses on five key building blocks for successful change:
- Awareness: Demonstrating to users and stakeholders why changes are necessary.
- Desire: Encouraging those who will be affected to get on board with the necessary changes. This can help people actively want changes instead of resisting.
- Knowledge: Providing information and training about the changes, such as using new technology.
- Ability: Ensuring healthcare professionals are equipped to use this new technology in real-world scenarios.
- Reinforcement: Making sure the change is sustained, refresher training is delivered as needed, and new approaches and technology are being used.
An example of this: Implementing an EHR system requires raising awareness about the system's benefits. This can encourage a desire for change among clinicians, providing training (knowledge). It can also keep staff using the system effectively (ability) and reinforcing its use through ongoing support.
Using the ADKAR model makes it easier whenever new technology is introduced.
-
The Kotter Change Management Model
Kotter's model emphasizes an eight-step process for change:
- Create Urgency: Explain why change is needed.
- Form a Powerful Coalition: A multi-stakeholder coalition is a powerful way to guarantee the change is implemented.
- Develop a Vision for Change: There must be a vision and strategy for the changes that are required.
- Communicate the Vision: It needs to be communicated effectively.
- Remove Obstacles: This could involve explaining how new technology could integrate with current systems, and where the budget will come from to pay for it.
- Create Short-term Wins: An ITIL approach is to start small, demonstrate how effective something is, and use it to achieve the short-term goal.
- Build on the Change: With a small trial, a larger roll-out is possible.
- Anchor the Changes in Culture: Training and awareness are now needed to embed these changes across the organization.
An example of this: A hospital transitioning to telehealth can create urgency by emphasizing patient demand for virtual care.
This has continued after the Covid-19 pandemic as it's proving more cost-effective and especially better for patients in rural communities. There could be coalitions of telehealth advocates anchoring the change by embedding telehealth in standard patient care protocols.
-
The McKinsey 7-S Change Model
This model aligns the following seven organizational elements to implement change effectively:
- Strategy
- Structure
- Systems
- Shared Values
- Style
- Staff
- Skills
An example of this: When introducing AI-driven diagnostic tools, the following provide for seamless integration:
- Aligning the strategy with patient care goals
- Training staff
- Adapting workflows
For more on the three above models, see our top 3 healthcare change management models blog post.
-
Electronic Health Record (EHR) Approach
Implementing or upgrading EHR systems enhances data accessibility, streamlines workflows, and improves patient care coordination.
But this isn't easy to do, especially when EHRs interact with so many other systems and data is so heavily regulated. Change management helps get clinician buy-in and minimizes workflow disruptions during adoption. -
Telehealth Digital Transformation
Telehealth adoption surged during the Covid-19 pandemic and continues to grow. Using this technology is especially useful for those in isolated, rural communities, or for those who can't easily come in to see their doctor.
Successful telehealth implementation change management addresses technical challenges, staff training, and patient education.
-
Digital Patient Intake Models
Automated patient intake processes reduce administrative burdens and enhance efficiency. Most healthcare providers have switched to these models. However, if your organization did this 10+ years ago, it could be time for an upgrade.
ITSM-led change management in patient intake models involves training staff and integrating digital tools into daily operations.
-
Using AI in Patient Diagnosis Processes
AI tools are becoming increasingly popular because they improve diagnostic accuracy and speed. However, you must be careful about picking the right ones and then rolling these out in the right way.
Effective change management brings trust to clinicians and the effective use of AI while maintaining patient-centric care.
-
Improving Patient-Centered Care
Change initiatives that prioritize patient-centered care can include personalized treatment plans or enhanced communication tools. It also may require staff engagement and cultural shifts. Make sure you have the right training and tools before launching any patient-centric initiatives.
-
Enhanced Approaches to Patient Safety and Risk Management
Adopting tools like predictive analytics for risk management requires alignment between IT, clinical teams, and leadership. Get buy-in early on from the relevant medical staff that will be affected. This can help make sure they're happy with any changes that impact how patients are looked after.
Have the relevant trials and risk assessments done before introducing anything new in this area.
-
Adapting to New Healthcare Regulations
Navigating regulatory changes, such as updated HIPAA requirements, involves clear communication, training, and process adjustments. There are countless ways technology, including AI, is making adapting to healthcare regulations easier, so these changes are usually welcomed more easily.
Now, let's look at the top 5 healthcare change management best practices that CIOs and healthcare leaders need to think about.
Top 5 Healthcare Change Management Best Practices
As we have seen from being involved with and supporting numerous healthcare change management initiatives, these best practices make the whole process easier and less painful for all parties:
- Engage Stakeholders Early: Include clinicians, administrators, and patients in planning and decision-making to build trust and minimize resistance. Trust is essential when patient safety and patient-centric procedures are concerned.
- Communicate Clearly and Frequently: Use multiple channels to explain the reasons for change, expected benefits, and progress updates. Get buy-in as early as you can and engage those who are resisting to understand why, and implement any feedback that makes sense.
- Provide Comprehensive Training: Ensure staff have the knowledge and skills needed to adopt new tools or processes effectively. Make it easier to encourage adoption with the right training at the right time.
- Small-scale, Pilot Changes: Start with small-scale implementations to gather feedback, address issues, and refine processes before full-scale rollout.
- Monitor and Support Staff: Offer continuous support through help desks, coaching, or follow-up sessions to reinforce changes and address challenges.
How to Measure Change Management in Healthcare
To assess the success of change management initiatives, healthcare organizations can use the following metrics:
- Adoption Rates: Percentage of staff using new systems or processes
- Training Completion Rates: Number of employees who completed training programs
- Feedback Scores: Employee and patient feedback on the changes
- Operational Metrics: Improvements in efficiency, such as reduced wait times or increased patient throughput
- Compliance Rates: Adherence to new regulations or protocols
- Patient Outcomes: Metrics like readmission rates or patient satisfaction scores
Of course, when technology is an integral part of treatment then there are going to be other scores and measures to consider. Patient survival rates, or test result scores compared to previous approaches need to be considered.
Key Takeaways: Streamlined Process for the Best Change Management in Healthcare
Change management in healthcare is essential to navigate the complexities of digital transformation, regulatory updates, and evolving patient needs.
Using models and frameworks can make change management in healthcare easier to manage, implement, and monitor the impacts and outcomes.
CIOs and digital leaders can drive successful change initiatives that improve patient care, operational efficiency, and organizational resilience. In most cases, change is for the better, providing patient outcomes improve, alongside greater operational efficiency, and handling regulatory burdens or other cost increases.
ITSM-based change management in healthcare can be a powerful catalyst for improvements that patients, healthcare organizations, and healthcare professionals need.
Other Useful Healthcare Change Management Resources
- Giva's HIPAA Resource Center for Healthcare Organizations
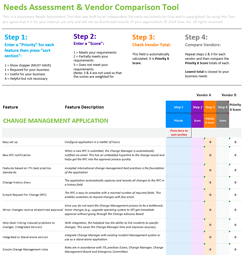
- How to Conduct an IT Change Management Software Needs Analysis (Including a Free Assessment Excel)
- ITIL-Aligned Standalone Change Management Software
- Compare the 20 Best IT Change Enablement/Management Solutions for 2025
- Giva's HIPAA Compliant Solutions for Healthcare
- Giva's Complete Guide to ITIL Change Management
Giva Helps Bring Change Management Success
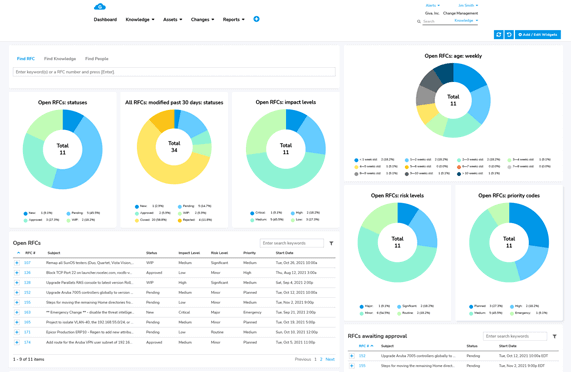
Giva's ITIL-Aligned Standalone Change Management Software can streamline your processes in the following ways:
- Quickly modernize IT processes
- Gain complete visibility with a centralized system of record, real-time dashboards and notifications
- Implement quickly with out-of-the-box ITIL defaults
- Ensure proper vetting and approval with established change control workflows
To learn more, book a free Giva demo to see our solutions in action, or start your own free, 30-day trial today!